Solutions

Solutions
Unified Threat Management
Intelligent Voice Automation
Conversational AI Voice Agent
Customer Intelligent E-Commerce
TikTok Micro-Influencer Marketing
Autonomous Penetration Testing

Insights
Explore in-depth articles for insights, research, and expert guidance on key industry topics.
Explore Insights
Get in Touch
Contact our sales team for product questions, pricing details, or tailored guidance.
Talk To SalesWhy HaloTree
Industries We Serve

Industries We Serve

Financial Services & Insurance

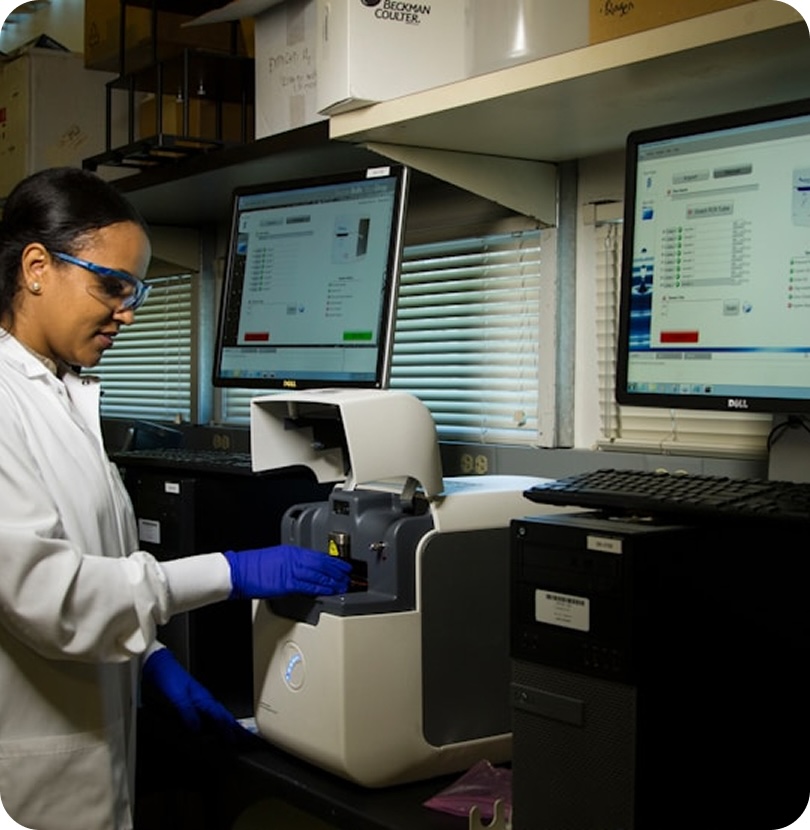
Healthcare & Life Sciences

Retail & E-Commerce

Collections & Receivables

Telecommunications

Government & Public Sector

Insights
Explore in-depth articles for insights, research, and expert guidance on key industry topics.
Explore Insights
Get in Touch
Contact our sales team for product questions, pricing details, or tailored guidance.
Talk To SalesCompany

Insights
Explore in-depth articles for insights, research, and expert guidance on key industry topics.
Explore Insights
Get in Touch
Contact our sales team for product questions, pricing details, or tailored guidance.
Talk To SalesInsights
Contact Us